Some notes on oxalic acid for foragers
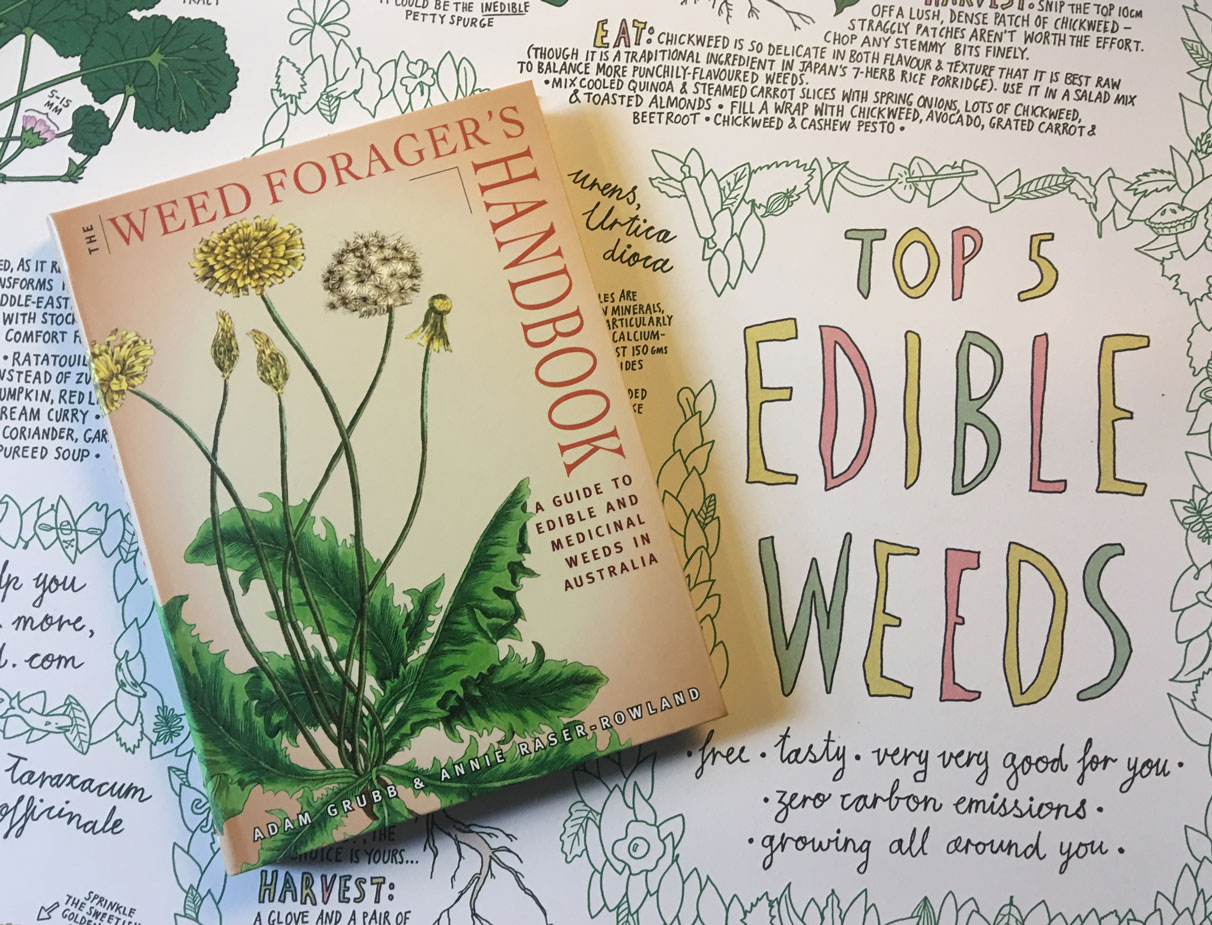
In writing The Weed Forager’s Handbook we took some deep dives into researching the potential health hazards related to foraging. Here is our fully-referenced extended remix of our information on oxalic acid. The version in the book is much shorter and gets more quickly to the relevant strategies.
In a nutshell, we don’t believe oxalic acid poses a serious health threat if you’re of normal health and reasonable about your consumption. While some wild foods are fairly high in oxalic acid, it’s certainly no reason not to forage, but it is worth knowing a little about it.
There are some easy strategies to allow you to take advantage of these free and nutritionally-rich plants – while not overdoing the oxalic acid.
If you want to skip straight to these, scroll down to ‘Strategies for eaters and foragers’ below. Otherwise, here’s our deep dive.
What is oxalic acid?
Oxalic acid (chemical formula H2C2O4) is a simple organic acid that occurs naturally in high levels in many common foods, including spinach, whole wheat, almonds, peanuts, beans, beets, rhubarb and chocolate.1“Oxalate Table | Nutrition Questionnaire Service Center.” 2022. Harvard T.H. Chan School of Public Health. June 23, 2022. https://www.hsph.harvard.edu/nutrition-questionnaire-service-center/nutrient-tables-download-page/2Massey, Linda K, Helen Roman-Smith, and Roger A. L Sutton. 1993. “Effect of Dietary Oxalate and Calcium on Urinary Oxalate and Risk of Formation of Calcium Oxalate Kidney Stones.” Journal of the American Dietetic Association 93 (8): 901–6. https://doi.org/10.1016/0002-8223(93)91530-4.
Oxalic acid is an anti-nutrient that can block the absorption of calcium, and it can also be a factor in kidney stone formation.
Most of the oxalic acid in our bodies doesn’t come from our diet though.
Oxalic acid is a byproduct of the normal human metabolism of vitamin C and collagen.3Crivelli et al., 2021. “Contribution of Dietary Oxalate and Oxalate Precursors to Urinary Oxalate Excretion.” Nutrients 13 (1): 62. https://doi.org/10.3390/nu13010062.
While generally considered merely a metabolic waste product, some researchers have suggested that oxalic acid may play some beneficial roles in the body.4Mahmut Çalişkan, “The Metabolism of Oxalic Acid,” Journal of Zoology 24 (2000): 103–106.5Albrecht, Steffen, Herbert Brandl, and Christoph Schönfels. “Human Oxalate—Really Just an End-Product of Metabolism?” Angewandte Chemie International Edition in English 33, no. 17 (September 16, 1994): 1780–81. https://doi.org/10.1002/anie.199417801.6Stewart Robertson, Daniel. “The Function of Oxalic Acid in the Human Metabolism.” Clinical Chemistry and Laboratory Medicine 49, no. 9 (January 1, 2011). https://doi.org/10.1515/CCLM.2011.238.
Oxalic acid forms various salts – known as oxalates – when it binds with minerals such as calcium, magnesium, sodium and potassium. We’ll refer to oxalic acid and its salts collectively as oxalic acid or oxalates somewhat interchangeably.
The important bit is that some of these oxalates (potassium and sodium) are soluble and are more likely to be absorbed by your gut, and some of these oxalates (calcium and magnesium) are insoluble, and pass straight through your digestive tract.7Lo, D., Wang HsinI, Wu WanJen, and Yang RayYu. 2018. “Anti-Nutrient Components and Their Concentrations in Edible Parts in Vegetable Families.” CABI Reviews 2018 (August): 1–30. https://doi.org/10.1079/PAVSNNR201813015.8Massey, Linda K. 2007. “Food Oxalate: Factors Affecting Measurement, Biological Variation, and Bioavailability.” Journal of the American Dietetic Association 107 (7): 1191–94. https://doi.org/10.1016/j.jada.2007.04.007.
Oxalic acid is widespread in plants, but some plants have much higher levels than others. The ratio of soluble to insoluble oxalates varies also.
What’s the relationship to foraging?
Many wild edibles are high in oxalic acid. These include amaranth (Amaranthus species), fat hen (Chenopodium album), dock (Rumex species), oxalis (Oxalis species), blackberry nightshade (Solanum nigrum), purslane (Portulaca oleracea) and to a lesser extent, Madeira vine (Anredera cordifolia) and chickweed (Stellaria media).9Guil, J., I. Rodríguez-Garcí, and E. Torija. 1997. “Nutritional and Toxic Factors in Selected Wild Edible Plants.” Plant Foods for Human Nutrition (Formerly Qualitas Plantarum) 51 (2): 99–107. https://doi.org/10.1023/A:1007988815888.10Noonan, SC, and GP Savage. 1999. “Oxalate Content of Foods and Its Effect on Humans.” Asia Pacific Journal of Clinical Nutrition 8 (1): 64–74. https://doi.org/10.1046/j.1440-6047.1999.00038.x.11Yimer, Abebe, Sirawdink Fikreyesus Forsido, Getachew Addis, and Abebe Ayelign. 2023. “Nutritional Composition of Some Wild Edible Plants Consumed in Southwest Ethiopia.” Heliyon 9 (6): e16541. https://doi.org/10.1016/j.heliyon.2023.e16541.12Tsai, Jeng-Yu, Jong-Khing Huang, Tony T Wu, and Ying Huei Lee. 2005. “Comparison of Oxalate Content in Foods and Beverages in Taiwan.”
The levels of oxalic acid in these wild plants are comparable to those in some widely eaten cultivated plants, including spinach, silverbeet, rhubarb and garden sorrel (see table below).
In this sense, foraging is not particularly more dangerous than browsing the vegetable aisle at the supermarket!
But that’s not to say browsing the vegetable aisle is entirely risk free, believe it or not. And the strategies we mention are of relevance to anyone’s diet, forager or not.
Besides total oxalate content, some plants which have a highly acidic sap, and a correspondingly tangy taste – such as sorrel, dock and oxalis – and tend to have a higher percentage of soluble oxalates. Whereas others with a more neutral sap and no tang to their taste – such as spinach, amaranth and fat hen – tend to have a lower percentage of soluble oxalates, although still significant.13Vityakon, Patma. 1986. “Effects of Environmental Factors on Nutrients and Antinutrient Contents of Selected Leafy Vegetables.” http://hdl.handle.net/10125/56468.
What are the concerns?
Anti-nutrient
In the diet, when oxalic acid binds with calcium and magnesium, it makes these minerals insoluble and unavailable to the body.14Bohn, Torsten, Lena Davidsson, Thomas Walczyk, and Richard F. Hurrell. 2004. “Fractional Magnesium Absorption Is Significantly Lower in Human Subjects from a Meal Served with an Oxalate-Rich Vegetable, Spinach, as Compared with a Meal Served with Kale, a Vegetable with a Low Oxalate Content.” British Journal of Nutrition 91 (4): 601–6. https://doi.org/10.1079/BJN20031081.15Bonsmann, S. Storcksdieck genannt, T. Walczyk, S. Renggli, and R. F. Hurrell. 2008. “Oxalic Acid Does Not Influence Nonhaem Iron Absorption in Humans: A Comparison of Kale and Spinach Meals.” European Journal of Clinical Nutrition 62 (3): 336–41. https://doi.org/10.1038/sj.ejcn.1602721. So for this reason, oxalic acid is described as an ‘anti-nutrient’. Spinach, for instance, while high in calcium, is not a great source of dietary calcium,16Noonan et al., 1999 and that’s true for some the above mentioned edible weeds also. As we’ll see below though, a little food combining can reduce concerns here.
Kidney stones
While there are different types of kidney stones, most (around 70-80%) are composed of calcium oxalate.17Massey et al., 1993
It’s normal that your kidneys will be processing both calcium and small amounts of oxalic acid simultaneously. Occasionally, these two substances can combine to form crystals. When there is a high level of oxalic acid and a low volume of urine, these crystals can further transform into stones.18Mitchell, Tanecia, Parveen Kumar, Thanmaya Reddy, Kyle D. Wood, John Knight, Dean G. Assimos, and Ross P. Holmes. 2019. “Dietary Oxalate and Kidney Stone Formation.” American Journal of Physiology – Renal Physiology 316 (3): F409–13. https://doi.org/10.1152/ajprenal.00373.2018.
Some people are more prone to kidney stones than others.
It’s not entirely clear how much dietary oxalic acid influences kidney stones, however, with some studies finding little to no relationship with dietary oxalic acid, and some studies finding that diets high in vegetables and nuts (and correspondingly oxalic acid) are associated with fewer kidney stones – probably due to complex dietary factors.19Petroski, Weston, and Deanna M. Minich. 2020. “Is There Such a Thing as ‘Anti-Nutrients’? A Narrative Review of Perceived Problematic Plant Compounds.” Nutrients 12 (10): 2929. https://doi.org/10.3390/nu12102929.
That said, it might still be a good idea you’ve ever had kidney stones, to limit the amount of high oxalate foods in your diet. High intake of vitamin C may also be a concern if you are prone to kidney stones.20Alessandra Calabria Baxmann, Claudia De O G Mendonca, and Ita Pfeferman Heilberg, “Effect of vitamin C supplements on urinary oxalate and pH in calcium stone-forming patients,” Kidney Int 63, no. 3 (March 2003): 1066-107121Traxer, Olivier, Beverley Huet, John Poindexter, Charles YC Pak, and Margaret S Pearle. 2003. “Effect of Ascorbic Acid Consumption on Urinary Stone Risk Factors.” The Journal of Urology 170 (2): 397–401.
Fatal poisoning
In high doses, soluble forms of oxalic acid can cause fatal poisonings, although from food sources this seems extremely rare.
There is however at least one recorded death from a high oxalic acid meal in the last 50 years. In 1989, a 53-year-old man (who had liver disease, diabetes, and was a heavy smoker and drinker) died after eating approximately 6-7 grams of oxalic acid in a soup containing around half a kilogram of sorrel. In the autopsy his liver, kidney and heart were all found to contain calcium oxalate crystals.22Farré, Mercè, Judith Xirgu, Antonio Salgado, Ramón Peracaula, Ramón Reig, and Pere Sanz. 1989. “Fatal Oxalic Acid Poisoning from Sorrel Soup.” The Lancet 334 (8678–8679) (December 30): 1524. doi:10.1016/S0140-6736(89)92967-X.
Note: The case record actually incongruently lists the ingredient as ‘sorrel’ but uses the botanical name ‘Rumex crispus’ which is the wild relative, curly dock.
The only other fatal case studies we could find reference are historical reports of children dying from eating rhubarb leaves. This suggests children may be more vulnerable to high oxalic acid foods.23Sanz, P, and R Reig. 1992. “Clinical and Pathological Findings in Fatal Plant Oxalosis: A Review.” The American Journal of Forensic Medicine and Pathology 13 (4): 342–45.
Kidney failure
There are some other cases of serious kidney issues. In Turkey in 2015, a child was hospitalised after a day eating large amounts of raw sorrel (Rumex acetosa), but fortunately made a full recovery 24Selçuk, Sinem Nur, Bora Gülhan, Ali Düzova, and Özlem Tekşam. “Acute Tubulointerstitial Nephritis Due to Large Amount of Sorrel (Rumex Acetosa) Intake.” Clinical Toxicology 53, no. 5 (May 28, 2015): 497–497. https://doi.org/10.3109/15563650.2015.1033061. and there are some reports of adults having temporary kidney failure after eating star fruit and some of it’s relatives due to the oxalic acid content.25Nair, Sreeja, Jacob George, Sajeev Kumar, and Noble Gracious. n.d. “Acute Oxalate Nephropathy Following Ingestion of Averrhoa Bilimbi Juice.” Case Reports in Nephrology.26Chen, Chien-Liang, Hua-Chang Fang, Kang-Ju Chou, Jyh-Seng Wang, and Hsiao-Min Chung. 2001. “Acute Oxalate Nephropathy After Ingestion of Star Fruit.” American Journal of Kidney Diseases 37 (2): 418–22. https://doi.org/10.1053/ajkd.2001.21333.
It’s rare, and probably exclusively associated with with the particular risk factors listed next – but high levels of consumption of oxalic acid can even lead to permanent kidney failure.
Cases of this have included when people with one or more of said risk factors adopted a diet based on juice or smoothies made from raw vegetables, or eaten excessive amounts of rhubarb for a period.27Getting, Jane E., James R. Gregoire, Ashley Phul, and Mary J. Kasten. 2013. “Oxalate Nephropathy Due to ‘Juicing’: Case Report and Review.” The American Journal of Medicine 126 (9): 768–72. https://doi.org/10.1016/j.amjmed.2013.03.019.28Makkapati, Swetha, Vivette D. D’Agati, and Leah Balsam. 2018. “‘Green Smoothie Cleanse’ Causing Acute Oxalate Nephropathy.” American Journal of Kidney Diseases 71 (2): 281–86. https://doi.org/10.1053/j.ajkd.2017.08.002.29Albersmeyer, Marc, Robert Hilge, Angelika Schröttle, Max Weiss, Thomas Sitter, and Volker Vielhauer. 2012. “Acute Kidney Injury after Ingestion of Rhubarb: Secondary Oxalate Nephropathy in a Patient with Type 1 Diabetes.” BMC Nephrology 13 (1): 141. https://doi.org/10.1186/1471-2369-13-141.
Risk factors
Those with a chronic kidney disease or a transplanted kidney, may be much more likely to be to suffer kidney issues from oxalic acids (or high vitamin C) consumption.30Getting et al., 2013
Additionally the following can all greatly increase oxalic acid absorption by the digestive tract, and you should limit your oxalic acid intake:
-
inflammatory bowel disease
-
pancreatic insufficiency
-
medications that block fat absorption
-
small-intestine bypass procedures
-
recent or extensive antibiotic use31Getting et al., 2013
How much does dietary oxalic acid intake contribute to the levels in our blood?
As mentioned, even if we don’t eat oxalic acid, our bodies create it internally. Oxalic acid is biosynthesised from vitamin C, collagen, some amino acids and other sources.32Crivelli et al., 2021
Most of the oxalic acid in our bloodstream comes from these internally-generated sources.
But there’s a bit of inconsistency in the science about how much dietary sources contribute to blood oxalic acid levels in healthy people.
Prior to 2001, the oxalate content in food was largely ignored, as it was widely believed that only around 10% of our blood’s oxalate content originated from dietary sources in normal circumstances.33Massey, 2007
This changed when a study found that urinary oxalate increased by around 50% with the addition of a 250 mg dietary supplement.34Holmes, Ross P., Harold O. Goodman, and Dean G. Assimos. 2001. “Contribution of Dietary Oxalate to Urinary Oxalate Excretion.” Kidney International 59 (1): 270–76. https://doi.org/10.1046/j.1523-1755.2001.00488.x. The study did use a highly soluble form of oxalic acid. Usually, the dietary forms of oxalic acid that we consume are poorly absorbed, with a bioavailability of 1–6%. Whereas in a pure soluble supplement form it is significantly higher,35Silberhorn, Eric M. 2005. “Oxalates.” In Encyclopedia of Toxicology (Second Edition), edited by Philip Wexler, 320–22. New York: Elsevier. https://doi.org/10.1016/B0-12-369400-0/01058-9.36Hanson, CF, VH Frankos, and WO Thompson. 1989. “Bioavailability of Oxalic Acid from Spinach, Sugar Beet Fibre and a Solution of Sodium Oxalate Consumed by Female Volunteers.” Food and Chemical Toxicology 27 (3): 181–84. and in one study it was around 2.5 times higher when compared to spinach.37Massey et al., 1993
Earlier studies had found that “in some cases, rhubarb, spinach, beetroot, peanuts, chocolates, and tea, taken in normal dietary quantities, raised urinary oxalate by twofold or more in healthy subjects.”38Massey et al., 1993
A 2013 study giving 600 mg / day oxalic acid in the form of 150 ml of rhubarb juice found the oxalic acid in subjects’ urine increase by 65%. 39Siener, Roswitha, Diana J. Bade, Albrecht Hesse, and Bernd Hoppe. 2013. “Dietary Hyperoxaluria Is Not Reduced by Treatment with Lactic Acid Bacteria.” Journal of Translational Medicine 11 (1): 306. https://doi.org/10.1186/1479-5876-11-306.
On the other hand, a 2008 study concluded “the impact of dietary oxalate on urinary oxalate appears to be small” after finding only about a 5% difference in urinary oxalic acid levels between those in the lowest and highest quartiles of oxalic acid consumption in their regular diets. They estimated that the high quartile consumed about 70% more oxalic acid than the lowest quartile, although with a lot of uncertainty.40Taylor, Eric N., and Gary C. Curhan. 2008. “Determinants of 24-Hour Urinary Oxalate Excretion.” Clinical Journal of the American Society of Nephrology 3 (5): 1453–60. https://doi.org/10.2215/CJN.01410308.
So none of this feels very definitive, but maybe we could say that in ordinary circumstances, most day to day changes in dietary oxalic acids tend to change the amount in a healthy person’s blood usually by around 5 or 10%, but if lots of oxalic acid is eaten without extra calcium, that amount may be significantly higher, even doubling or more. The latter is unlikely to be an issue on any particular occasion, but if it is maintained, over time it may increase the likelihood of kidney stones in sensitive people.
What are normal levels of oxalic acid intake?
Actual estimates of average oxalic acid in the diet are surprisingly hard to come by, but one very small – five person – US study found about 150 mg/day was the average with the range between about 45 and 350 mg/day.41Holmes, Ross P., and Martha Kennedy. 2000. “Estimation of the Oxalate Content of Foods and Daily Oxalate Intake.” Kidney International 57 (4): 1662–67. https://doi.org/10.1046/j.1523-1755.2000.00010.x. A study of kidney stone formers (who may have already been on low oxalate diets) found most patients were consuming within a 50 to 150 mg/day range.42Siener, Roswitha, Dagmar Ebert, Claudia Nicolay, and Albrecht Hesse. 2003. “Dietary Risk Factors for Hyperoxaluria in Calcium Oxalate Stone Formers.” Kidney International 63 (3): 1037–43. https://doi.org/10.1046/j.1523-1755.2003.00807.x. And a 1987 Japanese study reportedly found normal intake ranging from 70 to 920 mg/day, with vegetarians higher at between 80 and 2000 mg/day.43Ogawa, Yoshihide, Tomonori Miyazato, and Tadashi Hatano. 2000. “Oxalate and Urinary Stones.” World Journal of Surgery 24 (10): 1154–59. https://doi.org/10.1007/s002680010193.
By comparison, a one cup (30 g) serve of fresh spinach or amaranth would add about an extra 300 mg of oxalic acid to your diet.44“Making Spinach with Low Oxalate Levels : USDA ARS.” n.d. Accessed July 3, 2023. https://www.ars.usda.gov/news-events/news/research-news/2017/making-spinach-with-low-oxalate-levels/.45“FoodData Central.” n.d. Accessed July 3, 2023. https://fdc.nal.usda.gov/fdc-app.html#/food-details/168462/nutrients.
Strategies for eaters and foragers
Food combining
Foods high in both calcium and oxalic acid are less of a concern than those merely high in oxalic acid, since the calcium bonds with the oxalic acid in the gut, becoming insoluble.46Curhan et al., 1997 The gritty feeling you get in the mouth if you eat custard or milk after consuming rhubarb is this process of crystal formation in action. As we’ve mentioned, once crystals form, they become insoluble and they mostly pass harmlessly through us.
Purslane, dock, fat hen (and we suspect oxalis) have high oxalic acid to calcium ratios, as does rhubarb, spinach, warrigal greens, silverbeet, cocoa and cashews.47José Luis Guil et al., “Oxalic Acid and Calcium Determination in Wild Edible Plants,” J. Agric. Food Chem. 44, no. 7 (1996): 1821-1823.48Noonan, et al., 1999
Combining high oxalic acid foods with high calcium foods binds these soluble forms of oxalic acid to the calcium, making them insoluble. Yoghurt is a great combination food, and purslane tzatziki is a classic dip, and one in which most oxalic acid is harmlessly bound up.49Moreau, A.-G., and G.P. Savage. 2009. “Oxalate Content of Purslane Leaves and the Effect of Combining Them with Yoghurt or Coconut Products.” Journal of Food Composition and Analysis 22 (4) (June): 303–306. doi:10.1016/j.jfca.2009.01.013. (We even have a recipe for that in The Weed Forager’s Handbook.)
Cooking methods
Another method of limiting oxalic acid consumption is to blanch. Contrary to what some books say, cooking does not destroy oxalic acid. However, blanching your greens for a few minutes and disposing of the water leaches out roughly one third of the oxalic acid.50Shashi Kala Yadav and Salil Sehgal, “Effect of domestic processing and cooking on selected antinutrient contents of some green leafy vegetables,” Plant Foods for Human Nutrition (Formerly Qualitas Plantarum) 58, no. 3 (September 1, 2003): 1-11. That’s one third of total oxalic acid but most of the soluble oxalic acid. The insoluble oxalates that remain largely pass right through us. So although you may also lose some nutrients, we can recommend this method.
Probiotics
The naturally occurring gut bacteria Oxalobacter formigenes eat oxalates.51Troxel, S.A., and R.K. Low. 2003. “Intestinal Oxalobacter Formigenes Colonization in Calcium Oxalate Stone Formers and Its Relation to Urinary Oxalate.” Journal of Endourology 17 (3): 173–176.
Many antibiotics may kill these beneficial bugs, increasing the risk of kidney stones,52Tasian, Gregory E., Thomas Jemielita, David S. Goldfarb, Lawrence Copelovitch, Jeffrey S. Gerber, Qufei Wu, and Michelle R. Denburg. 2018. “Oral Antibiotic Exposure and Kidney Stone Disease.” Journal of the American Society of Nephrology 29 (6): 1731. https://doi.org/10.1681/ASN.2017111213. so if you’ve taken antibiotics and have these symptoms, you might consider consulting your doctor to see if specific Oxalobacter probiotics are available.
Fermented foods and off-the-shelf probiotics can help also. The common Lactobacillus acidophilus bacteria as found in yoghurt and sauerkraut can also break down oxalic acid.53Campieri, C., M. Campieri, V. Bertuzzi, E. Swennen, D. Matteuzzi, S. Stefoni, F. Pirovano, et al. 2001. “Reduction of Oxaluria After an Oral Course of Lactic Acid Bacteria at High Concentration.” Kidney International 60 (3): 1097–1105.54Lieske, J. C, D. S Goldfarb, C. De Simone, and C. Regnier. 2005. “Use of a Probioitic to Decrease Enteric Hyperoxaluria.” Kidney International 68 (3): 1244–1249. However experiments using isolated strains of probiotics have had mixed and mostly disappointing results.55Petrosky et al., 2020
Wild lacto-fermenting (by making kimchi or sauerkraut style ferments) some of your greens may or may not serve as a relevant probiotic – but it should reduce the levels of oxalic acid during the fermentation process.56Wadamori, Yukiko, Leo Vanhanen, and Geoffrey P. Savage. 2014. “Effect of Kimchi Fermentation on Oxalate Levels in Silver Beet (Beta Vulgaris Var. Cicla).” Foods 3 (2): 269–78. https://doi.org/10.3390/foods3020269.
Pick fresh looking healthy plants?
One foraging note is that oxalic acid tends to be in higher concentrations in plants during dry conditions.57Noonan, et al., 1999
How it relates to plant age is not so clear – in some plants such as spinach and beets there is an increase as they reach full size leaves, then a decrease as the leaves mature.58Kitchen, J., and E. BURNS. 2006. “The Effect of Maturity on the Oxalate Content of Spinach (Spinacia Oleraceae L.).” Journal of Food Science 30 (August): 589–93. https://doi.org/10.1111/j.1365-2621.1965.tb01807.x.59Simpson, Thomas S., Geoffrey P. Savage, Robert Sherlock, and Leo P. Vanhanen. 2009. “Oxalate Content of Silver Beet Leaves (Beta Vulgaris Var. Cicla) at Different Stages of Maturation and the Effect of Cooking with Different Milk Sources.” Journal of Agricultural and Food Chemistry 57 (22): 10804–8. https://doi.org/10.1021/jf902124w.
Strategies summarised
So in conclusion we suggest you:
- avoid high oxalic acid foods if you have any of the mentioned risk factors, but otherwise:
- not eat unreasonably huge quantities of high oxalic acid foods in one sitting,
- blanching and discarding water if you are eating high oxalate foods for extended periods,
- food combine high oxalic acid foods with high calcium foods,
- if you’ve had antibiotics, take probiotics and unpasteurised fermented foods to recolonise your gut,
- stay hydrated,
- eat a well-rounded healthy diet… in which weeds can play a starring role.
Level of oxalic acid in various foods
For your interest, below is a table with the results of tests on various vegetables and wild edibles for their oxalic acid content. The results are for total oxalic acid, and don’t specify what percentage of the oxalic acids are soluble and insoluble – so their health effects might be quite different.
In plants with a highly acidic cell sap, such as oxalis and some species of dock, oxalate exists primarily as the acid potassium oxalate. In plants with a cell sap only slightly acidic, such as fat hen and amaranth, it exists usually as a mix of the soluble sodium oxalate and the insoluble calcium and magnesium oxalates.60Noonan, et al., 1999
Different studies also report some wildly divergent figures. So who knows what to make of it all!?
|
Vegetable or Fruit |
Oxalic Acid Content as a percentage |
|||
|
USDA61USDA Nutrient Data Laboratory. “Oxalic Acid Content of Selected Vegetables.” National Agricultural Library. http://www.nal.usda.gov/fnic/foodcomp/Data/Other/oxalic.html |
Dr. Duke |
Litholink |
Guil et al. 62Guil, José Luis, María Esperanza Torija, Juan José Giménez, Ignacio Rodríguez-García, and Antonio Giménez. 1996. “Oxalic Acid and Calcium Determination in Wild Edible Plants.” J. Agric. Food Chem. 44 (7): 1821–23. https://doi.org/10.1021/jf950472a. |
|
| Amaranth |
1.09 |
— |
— |
0.96 |
| Beans |
0.36 |
0.03 |
0.02 |
— |
| Beets |
— |
0.04 |
0.68 |
— |
| Beet Greens |
0.61 |
— |
— |
— |
| Cabbage |
0.10 |
0.04 |
0.00 |
— |
| Carrots |
0.50 |
0.01 |
0.00 |
— |
| Celery |
0.19 |
— |
0.02 |
— |
| Chard, Swiss |
— |
— |
0.65 |
— |
| Chickweed |
— |
— |
— |
0.37 |
| Chicory |
0.21 |
— |
— |
— |
| Chives |
1.48 |
— |
0.00 |
— |
| Dandelion Greens |
— |
— |
0.02 |
— |
| Dock, Curly |
— |
— |
— |
0.62 |
| Kale |
0.02 |
— |
0.01 |
— |
| Fat Hen (Lambsquarters) |
— |
— |
— |
1.10 |
| Lettuce |
0.33 |
0.01 |
0.00 |
— |
| Mustard Greens |
— |
0.13 |
0.01 |
— |
| Parsley |
1.70 |
— |
0.10 |
— |
| Peas |
0.05 |
0.01 |
0.00 |
— |
| Peppers, Sweet |
0.04 |
0.12 |
0.02 |
— |
| Plantain, Broad Leaved |
— |
— |
— |
0.07 |
| Potatoes |
0.05 |
0.02 |
0.00 |
— |
| Purslane |
1.31 |
1.68 |
— |
— |
| Radishes |
0.48 |
0.01 |
0.00 |
— |
| Rhubarb (stems) |
— |
1.34 |
0.86 |
— |
| Sorrel |
— |
0.30 |
— |
— |
| Sow Thistle (S. tenerrimus) |
— |
— |
— |
0.06 |
| Spearmint |
— |
0.00 |
— |
— |
| Spinach |
0.97 |
0.66 |
0.68 |
— |
| Squash |
0.02 |
— |
0.02 |
— |
| Sweet Potatoes |
0.24 |
0.10 |
0.06 |
— |
| Tomato |
0.05 |
0.03 |
0.00 |
— |
| Watercress |
0.31 |
— |
0.01 |
— |
Hat tip to oxalicacidinfo.com for compiling the first three columns.63The Owlcroft Company. “Oxalic Acid and Foods.” http://oxalicacidinfo.com/.
To our knowledge, these are all fresh rather than dry weight figures.
Note that some of the food items mentioned in the opening paragraph was based on Harvard School of Public Health data64“Oxalate Table | Nutrition Questionnaire Service Center.” 2022. Harvard T.H. Chan School of Public Health. June 23, 2022. https://www.hsph.harvard.edu/nutrition-questionnaire-service-center/nutrient-tables-download-page/ which is published by serving size not by weight so we couldn’t include it in the table.
Disclaimer: we’re not medical professionals, we’re not scientists, we’re just foragers trying to figure out by reading the scientific literature to the best of our limited ability how to navigate this issue. Please don’t take any of this as medical advice, and particularly if you have any of the health issues mentioned, consult your doctor.
References
- 1“Oxalate Table | Nutrition Questionnaire Service Center.” 2022. Harvard T.H. Chan School of Public Health. June 23, 2022. https://www.hsph.harvard.edu/nutrition-questionnaire-service-center/nutrient-tables-download-page/
- 2Massey, Linda K, Helen Roman-Smith, and Roger A. L Sutton. 1993. “Effect of Dietary Oxalate and Calcium on Urinary Oxalate and Risk of Formation of Calcium Oxalate Kidney Stones.” Journal of the American Dietetic Association 93 (8): 901–6. https://doi.org/10.1016/0002-8223(93)91530-4.
- 3Crivelli et al., 2021. “Contribution of Dietary Oxalate and Oxalate Precursors to Urinary Oxalate Excretion.” Nutrients 13 (1): 62. https://doi.org/10.3390/nu13010062.
- 4Mahmut Çalişkan, “The Metabolism of Oxalic Acid,” Journal of Zoology 24 (2000): 103–106.
- 5Albrecht, Steffen, Herbert Brandl, and Christoph Schönfels. “Human Oxalate—Really Just an End-Product of Metabolism?” Angewandte Chemie International Edition in English 33, no. 17 (September 16, 1994): 1780–81. https://doi.org/10.1002/anie.199417801.
- 6Stewart Robertson, Daniel. “The Function of Oxalic Acid in the Human Metabolism.” Clinical Chemistry and Laboratory Medicine 49, no. 9 (January 1, 2011). https://doi.org/10.1515/CCLM.2011.238.
- 7Lo, D., Wang HsinI, Wu WanJen, and Yang RayYu. 2018. “Anti-Nutrient Components and Their Concentrations in Edible Parts in Vegetable Families.” CABI Reviews 2018 (August): 1–30. https://doi.org/10.1079/PAVSNNR201813015.
- 8Massey, Linda K. 2007. “Food Oxalate: Factors Affecting Measurement, Biological Variation, and Bioavailability.” Journal of the American Dietetic Association 107 (7): 1191–94. https://doi.org/10.1016/j.jada.2007.04.007.
- 9Guil, J., I. Rodríguez-Garcí, and E. Torija. 1997. “Nutritional and Toxic Factors in Selected Wild Edible Plants.” Plant Foods for Human Nutrition (Formerly Qualitas Plantarum) 51 (2): 99–107. https://doi.org/10.1023/A:1007988815888.
- 10Noonan, SC, and GP Savage. 1999. “Oxalate Content of Foods and Its Effect on Humans.” Asia Pacific Journal of Clinical Nutrition 8 (1): 64–74. https://doi.org/10.1046/j.1440-6047.1999.00038.x.
- 11Yimer, Abebe, Sirawdink Fikreyesus Forsido, Getachew Addis, and Abebe Ayelign. 2023. “Nutritional Composition of Some Wild Edible Plants Consumed in Southwest Ethiopia.” Heliyon 9 (6): e16541. https://doi.org/10.1016/j.heliyon.2023.e16541.
- 12Tsai, Jeng-Yu, Jong-Khing Huang, Tony T Wu, and Ying Huei Lee. 2005. “Comparison of Oxalate Content in Foods and Beverages in Taiwan.”
- 13Vityakon, Patma. 1986. “Effects of Environmental Factors on Nutrients and Antinutrient Contents of Selected Leafy Vegetables.” http://hdl.handle.net/10125/56468.
- 14Bohn, Torsten, Lena Davidsson, Thomas Walczyk, and Richard F. Hurrell. 2004. “Fractional Magnesium Absorption Is Significantly Lower in Human Subjects from a Meal Served with an Oxalate-Rich Vegetable, Spinach, as Compared with a Meal Served with Kale, a Vegetable with a Low Oxalate Content.” British Journal of Nutrition 91 (4): 601–6. https://doi.org/10.1079/BJN20031081.
- 15Bonsmann, S. Storcksdieck genannt, T. Walczyk, S. Renggli, and R. F. Hurrell. 2008. “Oxalic Acid Does Not Influence Nonhaem Iron Absorption in Humans: A Comparison of Kale and Spinach Meals.” European Journal of Clinical Nutrition 62 (3): 336–41. https://doi.org/10.1038/sj.ejcn.1602721.
- 16Noonan et al., 1999
- 17Massey et al., 1993
- 18Mitchell, Tanecia, Parveen Kumar, Thanmaya Reddy, Kyle D. Wood, John Knight, Dean G. Assimos, and Ross P. Holmes. 2019. “Dietary Oxalate and Kidney Stone Formation.” American Journal of Physiology – Renal Physiology 316 (3): F409–13. https://doi.org/10.1152/ajprenal.00373.2018.
- 19Petroski, Weston, and Deanna M. Minich. 2020. “Is There Such a Thing as ‘Anti-Nutrients’? A Narrative Review of Perceived Problematic Plant Compounds.” Nutrients 12 (10): 2929. https://doi.org/10.3390/nu12102929.
- 20Alessandra Calabria Baxmann, Claudia De O G Mendonca, and Ita Pfeferman Heilberg, “Effect of vitamin C supplements on urinary oxalate and pH in calcium stone-forming patients,” Kidney Int 63, no. 3 (March 2003): 1066-1071
- 21Traxer, Olivier, Beverley Huet, John Poindexter, Charles YC Pak, and Margaret S Pearle. 2003. “Effect of Ascorbic Acid Consumption on Urinary Stone Risk Factors.” The Journal of Urology 170 (2): 397–401.
- 22Farré, Mercè, Judith Xirgu, Antonio Salgado, Ramón Peracaula, Ramón Reig, and Pere Sanz. 1989. “Fatal Oxalic Acid Poisoning from Sorrel Soup.” The Lancet 334 (8678–8679) (December 30): 1524. doi:10.1016/S0140-6736(89)92967-X.
Note: The case record actually incongruently lists the ingredient as ‘sorrel’ but uses the botanical name ‘Rumex crispus’ which is the wild relative, curly dock. - 23Sanz, P, and R Reig. 1992. “Clinical and Pathological Findings in Fatal Plant Oxalosis: A Review.” The American Journal of Forensic Medicine and Pathology 13 (4): 342–45.
- 24Selçuk, Sinem Nur, Bora Gülhan, Ali Düzova, and Özlem Tekşam. “Acute Tubulointerstitial Nephritis Due to Large Amount of Sorrel (Rumex Acetosa) Intake.” Clinical Toxicology 53, no. 5 (May 28, 2015): 497–497. https://doi.org/10.3109/15563650.2015.1033061.
- 25Nair, Sreeja, Jacob George, Sajeev Kumar, and Noble Gracious. n.d. “Acute Oxalate Nephropathy Following Ingestion of Averrhoa Bilimbi Juice.” Case Reports in Nephrology.
- 26Chen, Chien-Liang, Hua-Chang Fang, Kang-Ju Chou, Jyh-Seng Wang, and Hsiao-Min Chung. 2001. “Acute Oxalate Nephropathy After Ingestion of Star Fruit.” American Journal of Kidney Diseases 37 (2): 418–22. https://doi.org/10.1053/ajkd.2001.21333.
- 27Getting, Jane E., James R. Gregoire, Ashley Phul, and Mary J. Kasten. 2013. “Oxalate Nephropathy Due to ‘Juicing’: Case Report and Review.” The American Journal of Medicine 126 (9): 768–72. https://doi.org/10.1016/j.amjmed.2013.03.019.
- 28Makkapati, Swetha, Vivette D. D’Agati, and Leah Balsam. 2018. “‘Green Smoothie Cleanse’ Causing Acute Oxalate Nephropathy.” American Journal of Kidney Diseases 71 (2): 281–86. https://doi.org/10.1053/j.ajkd.2017.08.002.
- 29Albersmeyer, Marc, Robert Hilge, Angelika Schröttle, Max Weiss, Thomas Sitter, and Volker Vielhauer. 2012. “Acute Kidney Injury after Ingestion of Rhubarb: Secondary Oxalate Nephropathy in a Patient with Type 1 Diabetes.” BMC Nephrology 13 (1): 141. https://doi.org/10.1186/1471-2369-13-141.
- 30Getting et al., 2013
- 31Getting et al., 2013
- 32Crivelli et al., 2021
- 33Massey, 2007
- 34Holmes, Ross P., Harold O. Goodman, and Dean G. Assimos. 2001. “Contribution of Dietary Oxalate to Urinary Oxalate Excretion.” Kidney International 59 (1): 270–76. https://doi.org/10.1046/j.1523-1755.2001.00488.x.
- 35Silberhorn, Eric M. 2005. “Oxalates.” In Encyclopedia of Toxicology (Second Edition), edited by Philip Wexler, 320–22. New York: Elsevier. https://doi.org/10.1016/B0-12-369400-0/01058-9.
- 36Hanson, CF, VH Frankos, and WO Thompson. 1989. “Bioavailability of Oxalic Acid from Spinach, Sugar Beet Fibre and a Solution of Sodium Oxalate Consumed by Female Volunteers.” Food and Chemical Toxicology 27 (3): 181–84.
- 37Massey et al., 1993
- 38Massey et al., 1993
- 39Siener, Roswitha, Diana J. Bade, Albrecht Hesse, and Bernd Hoppe. 2013. “Dietary Hyperoxaluria Is Not Reduced by Treatment with Lactic Acid Bacteria.” Journal of Translational Medicine 11 (1): 306. https://doi.org/10.1186/1479-5876-11-306.
- 40Taylor, Eric N., and Gary C. Curhan. 2008. “Determinants of 24-Hour Urinary Oxalate Excretion.” Clinical Journal of the American Society of Nephrology 3 (5): 1453–60. https://doi.org/10.2215/CJN.01410308.
- 41Holmes, Ross P., and Martha Kennedy. 2000. “Estimation of the Oxalate Content of Foods and Daily Oxalate Intake.” Kidney International 57 (4): 1662–67. https://doi.org/10.1046/j.1523-1755.2000.00010.x.
- 42Siener, Roswitha, Dagmar Ebert, Claudia Nicolay, and Albrecht Hesse. 2003. “Dietary Risk Factors for Hyperoxaluria in Calcium Oxalate Stone Formers.” Kidney International 63 (3): 1037–43. https://doi.org/10.1046/j.1523-1755.2003.00807.x.
- 43Ogawa, Yoshihide, Tomonori Miyazato, and Tadashi Hatano. 2000. “Oxalate and Urinary Stones.” World Journal of Surgery 24 (10): 1154–59. https://doi.org/10.1007/s002680010193.
- 44“Making Spinach with Low Oxalate Levels : USDA ARS.” n.d. Accessed July 3, 2023. https://www.ars.usda.gov/news-events/news/research-news/2017/making-spinach-with-low-oxalate-levels/.
- 45“FoodData Central.” n.d. Accessed July 3, 2023. https://fdc.nal.usda.gov/fdc-app.html#/food-details/168462/nutrients.
- 46Curhan et al., 1997
- 47José Luis Guil et al., “Oxalic Acid and Calcium Determination in Wild Edible Plants,” J. Agric. Food Chem. 44, no. 7 (1996): 1821-1823.
- 48Noonan, et al., 1999
- 49Moreau, A.-G., and G.P. Savage. 2009. “Oxalate Content of Purslane Leaves and the Effect of Combining Them with Yoghurt or Coconut Products.” Journal of Food Composition and Analysis 22 (4) (June): 303–306. doi:10.1016/j.jfca.2009.01.013.
- 50Shashi Kala Yadav and Salil Sehgal, “Effect of domestic processing and cooking on selected antinutrient contents of some green leafy vegetables,” Plant Foods for Human Nutrition (Formerly Qualitas Plantarum) 58, no. 3 (September 1, 2003): 1-11.
- 51Troxel, S.A., and R.K. Low. 2003. “Intestinal Oxalobacter Formigenes Colonization in Calcium Oxalate Stone Formers and Its Relation to Urinary Oxalate.” Journal of Endourology 17 (3): 173–176.
- 52Tasian, Gregory E., Thomas Jemielita, David S. Goldfarb, Lawrence Copelovitch, Jeffrey S. Gerber, Qufei Wu, and Michelle R. Denburg. 2018. “Oral Antibiotic Exposure and Kidney Stone Disease.” Journal of the American Society of Nephrology 29 (6): 1731. https://doi.org/10.1681/ASN.2017111213.
- 53Campieri, C., M. Campieri, V. Bertuzzi, E. Swennen, D. Matteuzzi, S. Stefoni, F. Pirovano, et al. 2001. “Reduction of Oxaluria After an Oral Course of Lactic Acid Bacteria at High Concentration.” Kidney International 60 (3): 1097–1105.
- 54Lieske, J. C, D. S Goldfarb, C. De Simone, and C. Regnier. 2005. “Use of a Probioitic to Decrease Enteric Hyperoxaluria.” Kidney International 68 (3): 1244–1249.
- 55Petrosky et al., 2020
- 56Wadamori, Yukiko, Leo Vanhanen, and Geoffrey P. Savage. 2014. “Effect of Kimchi Fermentation on Oxalate Levels in Silver Beet (Beta Vulgaris Var. Cicla).” Foods 3 (2): 269–78. https://doi.org/10.3390/foods3020269.
- 57Noonan, et al., 1999
- 58Kitchen, J., and E. BURNS. 2006. “The Effect of Maturity on the Oxalate Content of Spinach (Spinacia Oleraceae L.).” Journal of Food Science 30 (August): 589–93. https://doi.org/10.1111/j.1365-2621.1965.tb01807.x.
- 59Simpson, Thomas S., Geoffrey P. Savage, Robert Sherlock, and Leo P. Vanhanen. 2009. “Oxalate Content of Silver Beet Leaves (Beta Vulgaris Var. Cicla) at Different Stages of Maturation and the Effect of Cooking with Different Milk Sources.” Journal of Agricultural and Food Chemistry 57 (22): 10804–8. https://doi.org/10.1021/jf902124w.
- 60Noonan, et al., 1999
- 61USDA Nutrient Data Laboratory. “Oxalic Acid Content of Selected Vegetables.” National Agricultural Library. http://www.nal.usda.gov/fnic/foodcomp/Data/Other/oxalic.html
- 62Guil, José Luis, María Esperanza Torija, Juan José Giménez, Ignacio Rodríguez-García, and Antonio Giménez. 1996. “Oxalic Acid and Calcium Determination in Wild Edible Plants.” J. Agric. Food Chem. 44 (7): 1821–23. https://doi.org/10.1021/jf950472a.
- 63The Owlcroft Company. “Oxalic Acid and Foods.” http://oxalicacidinfo.com/.
- 64“Oxalate Table | Nutrition Questionnaire Service Center.” 2022. Harvard T.H. Chan School of Public Health. June 23, 2022. https://www.hsph.harvard.edu/nutrition-questionnaire-service-center/nutrient-tables-download-page/
- 65Harlow, Bernard L, Haim A Abenhaim, Allison F Vitonis, and Lisa Harnack. 2008. “Influence of Dietary Oxalates on the Risk of Adult-Onset Vulvodynia.” The Journal of Reproductive Medicine 53 (3): 171–78. [note: included this reference in 2023 when removing vulvodynia as a concern.]
[Edit 30 June 2023: I gave this page a pretty big overhaul, especially to mention risk factors to greater gut absorption which can lead to renal failure and other conditions, and give a more nuanced summary of the information on dietary intake and its effect on levels in the blood. Also added info about the acidity of certain weeds and the solubility of oxalic acid in them. Removed reference to a few health conditions that we previously thought might be affected by oxalic acid including vulvodynia65Harlow, Bernard L, Haim A Abenhaim, Allison F Vitonis, and Lisa Harnack. 2008. “Influence of Dietary Oxalates on the Risk of Adult-Onset Vulvodynia.” The Journal of Reproductive Medicine 53 (3): 171–78. [note: included this reference in 2023 when removing vulvodynia as a concern.] AG ]

0 Comments
11 Pingbacks